I'm taking the time to put up this page today because I just decided not to go in for my last qualifying exam for the CPA. I'll have another opportunity to take it next quarter, but I'm not prepared, in no small part because of this pregnancy.
I am not a doctor, just another pregnant woman with gestational diabetes, so please take any information presented here with a grain of salt.
Since I've been spending so much time dealing with the GD, I'm just hoping some of my experience might help other people in the same position. (All this reading and researching and testing has got to do somebody some good, right?)
DIAGNOSIS
They test you as part of your regular pregnancy checkups. My initial glucose tolerance test (isn't that orange drink nasty?) came back 174. They were looking for something under 140, so they called me back in for the more exhaustive 3 hour test. My scores were (fasting) 87, (1 hr) 184, (2 hr) 196, (3 hr) 153. That's a lot of FAIL. I had to go to the Diabetes Clinic and start seeing a specialist (endocrinologist) in addition to my regular OB/GYNE checkups.
TREATMENT
After they told me I was diabetic, it was 1.5 weeks before I was scheduled with the diabetes clinic. In the meantime, I overreacted and, for four days, CUT OUT ALL CARBS. OMG DO NOT DO THIS! For one, it makes you feel terrible. For another, it is also bad for the baby. If you aren't eating enough carbs, your ketones (and in my case, blood pressure too) go sky high.
On the first visit I met with the endocrinologist (who then left the country for the holidays for a month) and she asked me some questions about how I was feeling and gave me the speech about placenta blah blah, insulin resistance blah blah (check out the Mayo clinic site for those details). Then I met with the nutritionist, who told me when to eat how many carbs and gave me a couple of pamphlets with charts and whatnot. She gave some good advice (which I included under 'eating'). Her suggestion for appropriate, controlled carbohydrate ingestion was:
breakfast 30-40g carb
snack 10-20g carb
lunch 40-50g carb
snack 10-20g carb
dinner 45-60g carb
snack 10-20g carb
Then yet another person taught me how to use the glucose meter. I was very up front with them about my fear of needles and they seemed to hear that a lot. It turns out with the OneTouch UltraMini, it's sufficient to prick yourself on the forearm for the blood sample. This hurts a lot less than on the fingers, so if they don't suggest it when you go in, ask.
Then I saw another person, who administerd my A1C test. It looks at your red blood cells (another finger prick, one of the first in your upcoming stint as a pin cushion) and tells you what your average blood sugar has been over the last 3 months. I at first didn't see the point. It was already past, right? But when it came back in the normal range (5.8), it was very reassuring to know a) I haven't been diabetic all this time and they only just noticed, and b) no I wasn't poisoning my baby every time I had a dessert in the last three months.
That was it. I was given my chart to write my carbs and blood sugar results in and sent on my way with false hopes that I might be able to avoid the insulin injections altogether and manage this thing with diet (some people do).
I spent a few days carefully counting all my food and trying to eat the right numbers of carbs at the right times. When my numbers were still too high, I tried reducing the numbers of carbs per meal to get better results (and then add those carbs to snacks later on). I didn't think I was doing too badly. They want your fasting numbers to be <95 and your 2 hr post meal numbers to be <120. I was getting close to that most of the time. I faxed in my numbers, and apparently they didn't think they were good enough, because they left a message on my machine that I had to come in to talk to them about medication.
And I knew they meant insulin, and that meant injections. (If it were just some oral medication, they could phone it in to the pharmacy.) It was more FAIL. I followed all the rules and did what they told me, and it still didn't work. And now there were going to be injections. Lots and lots of injections. It was a good thing I was home alone at this point, because I wailed. I cried for a good couple of hours before I called them back and scheduled an appointment for that afternoon. I said to the nurse over the phone, "I didn't think the numbers were that bad." Maybe she heard the frustration or the previous 2hr crying jag in my voice, but she was quick to respond, "Oh no, they aren't *bad*. If you were a regular Type II diabetic, we would be patting you on the back. It's just that you're not. This is about the baby, and the standards are different."
They gave me two types of insulin pens. The kind they started me on right away is a fast-acting insulin I take before meals (in the Novolog Flexpen). The other one (the Lantus SoloStar pen), they just told me to hold on to for a bit. It's a longer, slower acting insulin. I had a foolish moment when I went to the pharmacy to pick up my Novolog pens. I told them I only wanted half the prescription because I had done the math on the dosages they had given me and there was no way I was going to even get to the second box of pens before I had this baby. Nobody warned me about how fast my insulin requirements were going to increase. When I started, one pen would have lasted a month. Right now, one pen might last me three days. I'm defnitely going to have to go back for the second half of that prescription, and then some.
I started on the long-acting insulin when my fasting glucose (first thing in the morning, before eating) got consistently above 95, only two weeks after starting with the fast-acting insulin.
I think my insulin requirements have shot up astonishingly fast, but noone at the diabetes clinic will confirm or deny that my course has been unusual. Mostly they skirt the issue and reassure me that this will all be over in just a few weeks when the baby is born. Still, it's very frustrating when no dose works two days in a row. You have to guess, and my chart is full of missed blood sugar readings (more FAIL) when I didn't increase the dosage enough. (But hey, the baby looks great, so maybe it's more about the consistency of the attempt at control.) I've included my chart in the next column, as an anecdotal example of one person's actual results. Like I said, I am not a doctor. I don't know if this is normal, or if your course of insulin would be steeper or less than my own. I can just tell you that it's real results.
I had to adjust my dose constantly, and couldn't be calling the clinic every day, so I asked for some general guidelines from them. In response to my concern that I was taking *a lot* of insulin, they replied that the only such thing as too much insulin was if my blood sugar got too low. If it went below 70 after a meal, I should back off on the insulin and have some glucose tablets or a snack (mostly I aim for ~110, just under the 120 target). If it went as high as 200, I should call the clinic right away. Also, there's some subtlety. I require twice the ratio of insulin/carb for breakfast than I do for lunch or dinner, so consult your blood sugars closely.
A note on KETONES
They also gave me some ketone strips to pee on every morning. When you fast overnight and your body isn't managing its blood glucose very well, you start to mobilize fat stores. This produces a side product of ketones, which will pass through the placenta to the baby. Ketones have been associated in at least one study with lower IQ in babies, so everyone is playing it safe and trying to reduce them. When they initially told me to start on the insulin, they said I wouldn't have to test for ketones any more. I DID ANYWAY, because, heck, I had paid for all those ketone strips so why not. I still had high ketones in the morning, and no matter how many carbs I tried to jam down for dinner (their proposed solution was to eat ~5-10 more g carbs with each meal), the morning ketone count was still high. What works, is setting an alarm for 3a.m., rolling over and grabbing 20g carbs of a LUNA snack bar (about 2/3 of a bar), and scarfing it down before going back to sleep. I've seen on the internet where some doctors recommend a glass of milk in the middle of the night, but that involves going all the way downstairs to the refrigerator. No thanks.
FOLLOW-UP
Something else nobody warned me about is that, when I went on insulin, the OB/GYNE office increased my checkups from once every two weeks to twice a week (completely separate from any additional appointments I might have at the diabetes clinic). This is a huge time committment, especially since everyone and their sister seems to be having babies right now, and I can never get in when my appointment is actually scheduled.
Once a week is an ultrasound, where they see if the baby is active, doing her practice breathing, and how big she's getting (44th percentile as of week 35, so not huge with glucose). She's been getting a health score of 8 out of 8 so far. The other time a week is an NST (non-stress test), in which they lie you down in a comfy recliner, and strap two sensors to your belly. One monitors your uterus for contractions. (They tell me I'm having contractions during this test, but I can't feel them. Apparently this is normal for this point in the pregnancy.) The other monitors your baby's heart rate. They take readings for about 20 minutes, looking for a baseline and at least two periods of activity where her heart rate increases. My girl baby has a baseline heart rate in the high 130s these days (week 35), down from 150s a month or so ago. And she likes to kick the sensors. They like the active babies, so she's doing well on these tests too. They also take your blood pressure a lot. GD puts you at higher risk for preeclampsia. The Mayo clinic can describe that better. A lot of the symptoms are similar to regular pregnancy side effects, which is why they monitor you so closely at this point. Just keep in mind that you're considered high risk now, and should communicate these things to your OB rather than write them off. I've had one bad headache with visual 'sparkles' (which I almost didn't mention, because I thought it was just a migraine that never fully materialised), and at least one blood pressure spike at 140, but for the most part am devoid of preeclampsia symptoms (my blood pressure since then has been in the low 120s).
WEB RESOURCES
(There's a bunch of wacky stuff on the internet. Be picky.)
Mayo Clinic
I almost always end up here when I'm researching medical conditions on the web. They're very clear and have a lot of reassuring detail. Put 'gestational diabetes' in the little search window.
Calorie King
The nutritionist pointed this one out. Type in anything and it will give you the carb count! Very handy.
EATING
Your nutritionist will give you a lot of literature, which will be overwhelming. I was terrified of food for the first week and a half, but you learn and you get into habits pretty quickly. There are a couple of tips that have really stuck with me.
- Always eat protein and/or fiber with your carbs.
- Fruit is good for you, but not in the morning.
- Meat, cheese, and *some* veggies are free foods. Stock up. (It's a relief to have food around that you don't have to count or agonize over.)
- Forget the desserts. Yes, you could count them and take the insulin, but there goes your whole meal, and it's still only a small portion.
- Chinese food is mysteriously non-diabetic friendly, no matter what the actual carb count. Avoid.
Snacks and foods I have found satisfying and convenient:
- a small (4oz) apple (15 carbs) and cheddar (0 carbs, but good protein to pair with your fruit)
- 1/2c cottage cheese (4 carbs) with 1c strawberries (11 carbs)
- milk - 13 carbs per cup, good for pregnant women, and scalable to fill out snacks and meals to the right carb count
- 1/4c peanut butter (12 carbs - but check the label, some add more sugar) and celery (0 carbs)
- Almonds (20 almonds=5g carbs, that's a lot of nuts)
- Baby carrots (1 carrot = 1g carb)
- Stouffers - good ingredients with the carb count right on the box (in about your target range).
Eating Out:
- Unfortunately, it's easier to eat out at a big chain. You can usually get the carb count for their menu online and plan ahead for what you are going to order. Pick a couple of things in case they are out.
- Subway's 6" sub is ~45g carbs, mostly from the bread, and then the fillings are usually negligible, and the info is posted right there in the store. They get mucho points for this.
- Steakhouse and diner cheeseburgers without ketchup (mayo and mustard are free, and most veggie toppings are negligible) are reliably ~45g carbs (from the bun). (Not McDonald's or Burger King, though, they put something carby and mysterious in their sauces.)
- I've been carrying a cup measure with me, so I can compare unknown portion sizes with the charts the nutritionist gave me. It makes restaurant people nervous when you start measuring their food, so you might want to briefly explain if they start frowning at you.
- When eating at a friend's, let them know that simple is better. Sauces should be on the side. If the ingredients are separate (ex. pot roast rather than meatloaf (which usually has bread crumbs in it)), then it's easier for you to figure out how many carbs you are eating. If they save the packaging for rolls and things, even better. You can even volunteer to make the carby dish.
- When going to a party at someone else's house, bring snacks that *you* can eat, and share them with other people (a nice meat, cheese, and almond platter for example).
MY INSULIN HISTORY
My required insulin dose has risen alarmingly in just a couple of weeks. This may or may not be typical, so make of it what you will. This chart was posted at the end of gestation week 35, and I am told that I could see some improvement in weeks 36-38, as the placenta eases off on some of its hormone production in preparation for birth.
Note that breakfast requires a much higher insulin dose per carb than either lunch or dinner, so the same dose for every meal might not be appropriate for you, either. Keep an eye on your chart. A ratio of 1 means I'm taking 30 units of insulin for my 30g carb breakfast at 35 weeks. The ratio of 0.5 means I'm taking 30 units of insulin for my 60g carb dinner at 35 weeks.
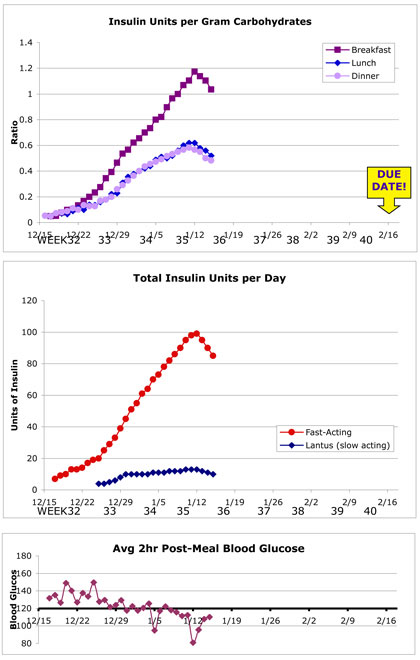
It looks like a lot of insulin to me... only a few more weeks, though.
Christmas was rough, not because I ate too much (I didn't), but because I had a vicious cold, which will also mess with your blood sugar.
GOOD THINGS to come out of this
- Possible reduction of needle phobia (jury's still out).
- Less pregnancy weight gained (in a healthy way, not a bad-for-the-baby kind of way).
- More nutrition knowledge in general.
- Better eating habits (smaller meals, better variety, less dessert).
- More baby bonding in ultrasound sessions.
- Getting to know the OB/GYNE staff better before birth.
- Better understanding of dietary requirements and concerns of diabetic friends.